Governments around the world continue to focus their attention on the COVID-19, communicable disease while ignoring the dangers that non-communicable diseases such as cancer, diabetes, hypertension, obesity, heart, and respiratory ailments pose to health.
Ghana too has prioritized fighting the virus but has paid scant attention to those who are at high risk of poor outcomes if they are infected with the virus people living with NCDs.
NCDs kill more than 41 million people each year. Some 80% of all NCD deaths occur in low- and middle-income countries. In Ghana, non-communicable diseases account for 43% of all deaths.
The major NCDs in Ghana are cardiovascular diseases, cancers, diabetes, chronic respiratory diseases, and sickle cell disease. Many NCDs are preventable and premature.
The common risk factors are tobacco use, harmful use of alcohol, unhealthy diet and physical inactivity.
In 2008, the World Health Organisation estimated that 36.4 percent of Ghanaians were hypertensive, 8.8 percent were diabetic, 17.6 percent had high cholesterol, and 36.4 percent were either overweight or obese.
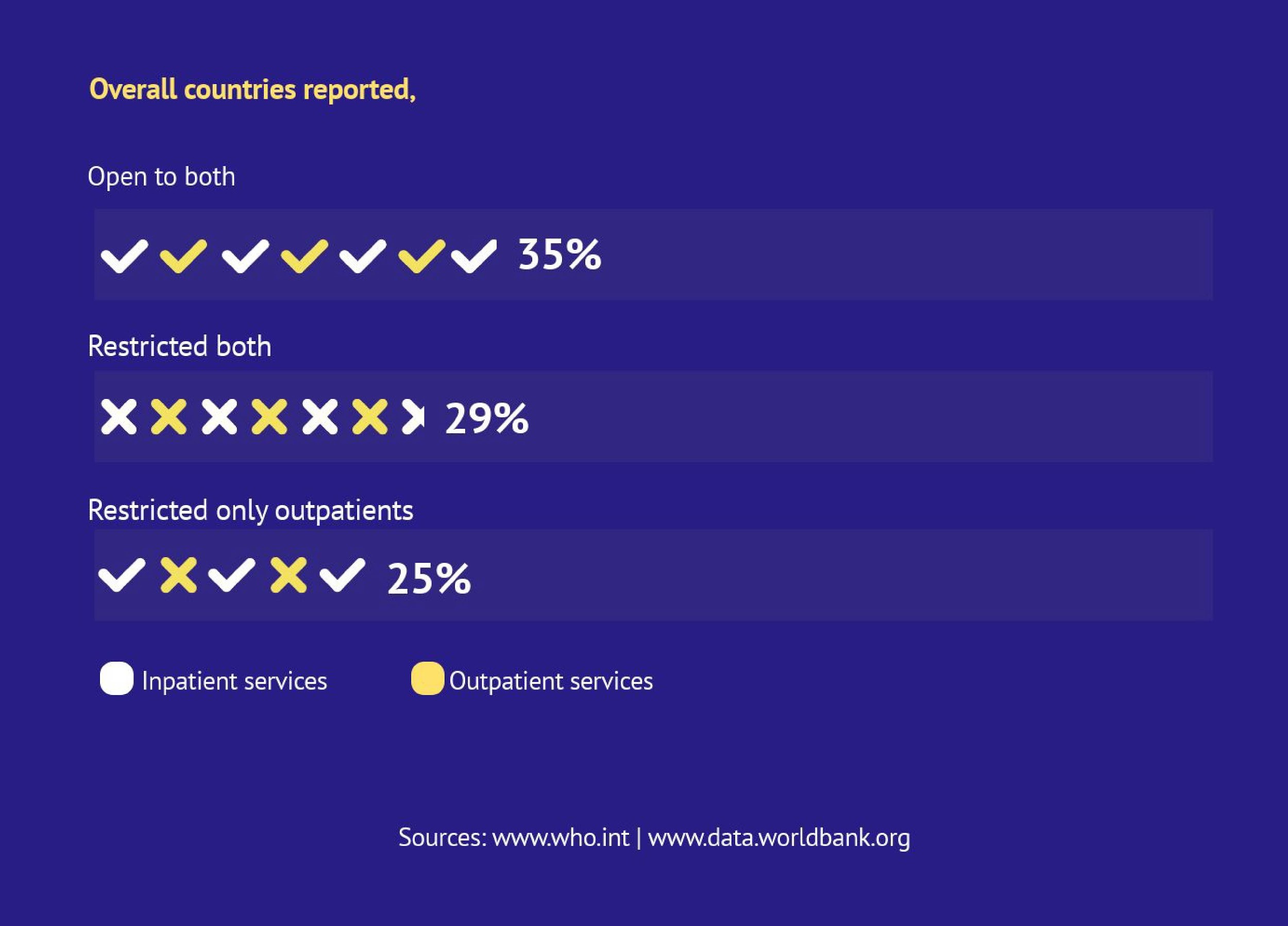
Accessing NCD prevention and care services was difficult before COVID-19 and has become nearly impossible since March. It also means that many people with these underlying health conditions are more vulnerable to the COVID-19 virus.
According to WHO, the majority of the 15 million people who die from NCDs are aged between 30-69 years. Those who have died from COVID-19 are also in this age group.
Amma Quaynoo, a journalist in the capital of Ghana’s Ashanti region does not abuse alcohol, tobacco and observes a healthy diet. She also tries to keep active.
But she suffers from Sickle Cell Disease, a group of disorders that affects hemoglobin, the molecule in red blood cells that delivers oxygen to cells throughout the body.
Sickle Cell disease is characterized by a change in the shape of a red blood cell, from a smooth circular shape to a crescent shape, which can result in the blockage of small blood vessels.
Every year, between 300,000 and 400,000 children are born with SCD; 75 percent of them (an estimated 240,000) in sub-Saharan Africa. The disease is genetic and causes health problems such as anaemia, episodic pain, swelling of the hands and feet and because it affects the spleen, many of those affected are at higher risk of infections.
Those affected by Sickle Cell Disease can experience shortness of breath and fatigue which are also among the symptoms of COVID-19. Those affected by SCD are also at higher risk of becoming infected with COVID-19.
Sadly, between 50 and 80 percent of these children die before their fifth birthday. The recurrent pain and complications caused by the disease can interfere with many aspects of the patient’s life, including education, employment and psychosocial development.
Recognising that her pre-existing condition placed her at high risk of contracting the novel coronavirus, Amma was quick to observe the frequent handwashing, physical distancing and mask-wearing guidelines issued by the government.
She was also lucky she had enough hydroxyurea, the medicine she has been prescribed to deal with the disease.
“At one point during the early months of the virus spread, the hospital where l got my medicine had to close when four of the nurses there contracted the virus.
Imagine if you were supposed to go for your checkup and your medicines? If you are on hydroxyurea, when it’s finished, you need to quickly go for a refill. They mix it in the hospital for you. You cannot mix it yourself in the house!”
Amma is concerned that the government has shown no interest in providing health services for people like her who suffer from sickle cell disease and other NCDs.
“They think it’s not as serious as COVID 19 but it is serious. Day in and day out people are dying from diabetes and its effect. People are dying from hypertension, people are getting strokes; People are dying from various cancers!”
Similar concerns have been expressed by the Ghana Non-Communicable Diseases Alliance, a network of Non-Governmental Organizations working in diverse areas of health and development. The network was established due to the rising health burden associated with NCDs in Ghana.
Network chairperson, Dr Beatrice Wiafe-Addai thinks too much attention has been given to the COVID-19 to the detriment of other diseases that are killing more people than the novel coronavirus.
She says that there has been a severe disruption in the delivery of chronic care, supplies of medicines and limited access to resources including health workers and support services for the management of NCDs.
With the focus on COVID-19, the usual screening of patients for NCDs, the nutrition clinics for those who are obese, chemotherapy for cancer patients and the provision of life-saving medicines such as Insulin for those with diabetes has been disrupted.
She is also concerned that due to the disruption of routine services such as NCD screening and diagnosis, people are more likely to present themselves with symptoms of more advanced diseases such as later-stage cancers (which are harder to treat), uncontrolled hypertension, chronic kidney disease. This will have an impact on the country’s health services that are already under-resourced.

“There’s a rise in the complications from non-communicable disease. There is a rise in the late case presentation of the cases. Most of our hospitals have been turned to COVID-19 centres. Some centres were turning patients away.
There was that scare that If you’re not careful you’d go and contract the disease from the hospital. So then someone who has breast cancer would rather stay in the house and wait. Mind you the time that she found her lump is not when it started. It could have been there for some time,” Dr Wiafe-Adda says.
Leticia Akyaah Boakye is a breast cancer survivor. Before COVID-19 spread globally and in Ghana, she would visit the hospital regularly for checkups and pick up her medication as well. However, she tells me how the private facility she visits has since improved its work processes to keep giving hundreds of patients the needed care.
This approach according to her was adopted because of the fear of contracting the virus.
“Some of the members of an association I’m part of kept calling me.They were not sure whether they would get their medicines or were free to go to the hospital. We kept calling some of the Doctors and nurses because they(breast cancer patients) were afraid, but they were assured there is no cause for alarm.
The Peace and Love Hospital has been providing patients like Boakye with medicines. Instead of them going to the hospital, the health personnel have been delivering the medicines to the patients’ homes. “They had our contacts, so they delivered to our homes at no extra cost!,” she said. She hoped that the government and other private hospitals will adopt this method to provide medicines to other patients like her who are vulnerable to contracting the virus or who are unable to visit the hospitals to collect their medicines.
In a survey organized by the Ghana Non-Communicable Diseases Alliance Network,the 127 respondents with different NCDs recommended that special arrangements be made for persons with NCDs who require constant medication to reduce the risk of getting infected with COVID-19 in long hospital queues at the out-patient departments of the health facilities.
They also suggested that the government establishes separate health care services in the form of mobile clinics or NCDS/diabetes clinics to cater for the needs of people with these underlying health conditions.
An estimated 22,823 new Cancer cases are reported every year in Ghana. The most prevalent cancer is prostate and breast cancer in males and females respectively. Public hospitals offer specialised oncology services include Korle-Bu and the Komfo Anokye Teaching hospitals.
Globally, 175 million adults are estimated to live with undiagnosed diabetes and over 1 billion people suffer from uncontrolled hypertension. The prevalence of diabetes among adults in Ghana is estimated at 1.8% (281,100 people) according to the International Diabetes Federation. They too may be at particularly high risk from COVID-19.
Unlike in many countries across the globe, the current death rate from Covid-19 is low. This is something the government of Ghana has taken credit for citing the restrictions it initiated immediately after the first case was reported in March.
On September 24, the government extended by three months the restrictions requiring the mandatory wearing of face masks in public, the closure of public spaces such as beaches and cinema halls as well as the closure of borders with other countries.
A system introduced by the information ministry where Ghanaians were informed periodically on measures taken by the government.
Although many people have welcomed the government’s intervention and decisions made to curtail the spread of COVID-19, they want attention to be given to NCDs to help reduce the rate at which people are contracting or getting ill from NCDs.
The World Health organization indicates that 71% of all global deaths (annually) is attributed to non-communicable diseases. Fifteen million people (between the ages of 30-69 years ) in low and middle-income countries (Ghana inclusive)die every year from NCDs.
The Chairperson of the Ghana Non-Communicable Diseases Alliance Network, Dr Beatrice Wiafe tells me how the rise of NCDs is problematic.
As a breast cancer advocate, she says COVID-19 worsened the plight of patients with non-communicable diseases. She is at the forefront of fighting breast cancer in Ghana which is still the most commonly diagnosed cancer in women.
As at October 6, there had been 46,829 reported cases of COVID 19 and 303 deaths. Pre-existing medical conditions such as obesity, Obesity, hypertension, diabetes all make someone susceptible to catching the novel coronavirus.
Public health advocacy groups and community-based organisations have been engaging in public awareness campaigns to educate and urge people to go to hospital for early detection of these diseases.
The public health officer in charge of the outpatient’s department at Korle-Bu teaching hospital, Regina Mireku said there was a high number of hypertension and diabetes cases recorded on a monthly basis.
“We have what we call the top ten. And always hypertension and diabetes are always the leading cases that come here in a month. And at the end of the year, it’s also the same. We see like two thousand to three thousand cases a month and because of our lifestyles and others, most of the referrals are based on hypertension.
Korle-bu is a teaching hospital and most of the patients who go here are referred there to attend the specialty clinics here. The numbers are increasing and we always educate them on adherence to their medication because some people do think that the diseases are hereditary”.
Samuel Sedodo is a stroke survivor. A stroke occurs when a blood vessel that carries oxygen and nutrients to the brain is either blocked by a clot or bursts (or ruptures). He lives in Peki, a town in the South Dayi district of the Volta Region. He survived a stroke over 15 years ago. He’s been in and out of the hospital for check-ups.
But even at the hospital, he has had to deal with the stigma from health workers who know enough about how the virus is spread but who are still concerned about their own safety.
They know that because of my condition, l am vulnerable to catching corona. They do not feel safe when attending to me or other patients at the NCD clinic. They are very abrupt and just want to finish with you quickly so that you can leave. It is not like before when they showed more concern,” he says.
While the Ghanian government works to ensure that the country attains a “COVID-19 free” status, state health efforts need support to ensure that Ghana’s NCD burden doesn’t get higher.
Those suffering from Sickle Cell Disease, Cancer, Diabetes, High Blood pressure and other NCDs are still getting medication and treatment especially through this pandemic where their illnesses put them at risk for poor outcomes if they do contract COVID-19.
—-
This report was supported by the Africa Women Journalism Project (AWJP) in partnership with the International Center for Journalists (ICFJ).